Day 1 :
- Anatomical Pathology | Oncology | Clinical Pathology | Clinical Oncology | Dermatopathology | Hematology Oncology | Cancer Stem Cells | Molecular Pathology | Cancer Diagnostics | Gastrointestinal and Liver pathology | Pediatric Oncology | Hematopathology | Radiation Oncology | Surgical Pathology | Cancer Biomarkers | Cytopathology and Histopathology | Oncology Case Reports | Breast Pathology | Renal and Urinary tract Pathology | Cancer Pharmacology | Oral and Maxillofacial Pathology | Cancer Research | Pulmonary Pathology | Microbial Pathology | Chemotherapeutic | Digital Pathology and e-Pathology | Cancer Therapy | OncoGenomics | Veterinary Pathology |
Session Introduction
Weibiao Cao
Rhode Island Hospital and Brown University, USA
Title: Mechanisms of the progression from Barrett’s esophagus to esophageal adenocarcinoma: role of NADPH oxidase NOX5-S

Biography:
Dr. Cao obtained his MD degree from Zhejiang Medical University in Hangzhou, China in 1986. Dr. Cao worked as a research associate and an assistant professor in Division of Gastroenterology, Rhode Island Hospital, RI, USA from 1996 to 2007. He was trained as a pathology resident from 2007 to 2011and a GI pathology fellow from 2011 to 2012 in the Department of Pathology, Rhode Island Hospital and Brown University, USA. Dr. Cao has been an attending pathologist since 2012, an associate professor since 2013 and a director of autopsy service since 2017 in Department of Pathology, Rhode Island Hospital and Brown University, USA. Dr. Cao has been a Member of Oncology C (ONCC) scientific peer review panel, Department of Veterans Affairs, USA and an editorial board member of Scientific Reports (impact factor 4.26) since 2015.
Abstract:
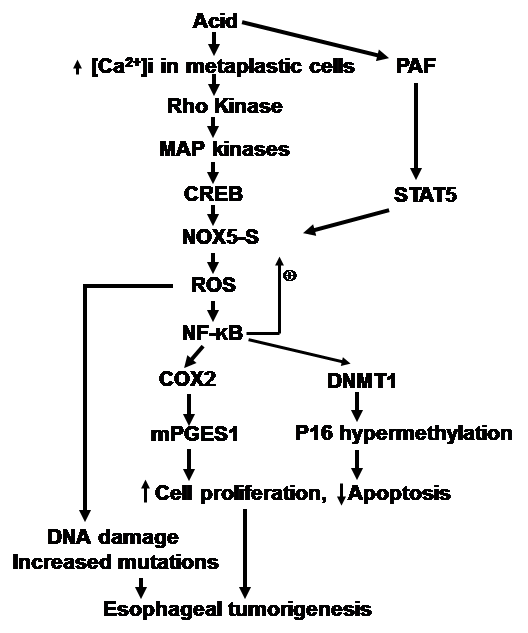
Esophageal adenocarcinoma (EA) has increased in incidence over the past several decades and is characterized by a poor prognosis. Gastroesophageal reflux disease (GERD) complicated by Barrett’s esophagus (BE) is a major risk factor for the development of EA. There is a progression from BE to dysplasia and to EA. However, the mechanisms of progression from BE to EA are not fully understood. We found that NOX5-S is present in Barrett’s cells BAR-T and EA cells FLO and OE33 and is overexpressed in FLO cells and EA tissues. NOX5-S mRNA is also increased in Barrett’s mucosa with high-grade dysplasia. Pulsed acid treatment significantly increases NOX5-S expression and H2O2 production in BAR-T and OE33 cells and Barrett’s mucosa. These data suggest that NOX5-S may be a source of overproduction of reactive oxygen species (ROS) in BE and in EA cells. We also found that acid-induced increase in NOX5-S expression may depend on activation of Rho kinase, ERK1/2 MAP kinases, and cAMP response element-binding protein. An acid may also induce production of platelet-activating factor, which activates signal transducer and activator of transcription 5 (STAT5) and then upregulates NOX5-S. In addition, NOX5-S mediates acid-induced increase in cell proliferation in Barrett’s cells BAR-T and EA cells (OE33 and FLO). NOX5-S-mediated increase in cell proliferation may depend on activation of COX2 and microsomal prostaglandin E synthase 1 (mPGES1), and downregulation of p16 via promoter methylation. NOX5-S also mediates acid-induced DNA damage. These data suggest that persistent acid reflux present in BE patients may upregulate NOX5-S, increase production of ROS and cell proliferation, and cause DNA damage, thereby contributing to the progression from BE to dysplasia and to EA.
Mitzli X. Velasco
National Autonomous University of Mexico, UNAM
Title: Antagonism between the RNA binding protein Musashi1 and miR-137 and its potential impact on neurogenesis and glioblastoma development

Biography:
Mitzli Xochitl Velasco López is a Ph.D. student of the Biomedical Sciences Program, The National Autonomous University of Mexico (UNAM), under the advice of Greco Hernández, of the Translation and Cancer Lab at National Institute of Cancer (INCan), Mexico City. She has done a research stay in the Lab of Luiz Penalva, University of Texas. Her research is focused on the study post-transcriptional mechanisms involved in cancer development. She is studying how RNA-binding proteins and microRNAs are involved at the interesting intersection between neurogenesis and brain tumor development, especially in glioblastoma.
Abstract:
In the last decade, an ever-growing number of connections between microRNAs (miRNAs) and RNA-binding proteins (RBPs) has uncovered a new level of complexity of gene expression regulation in cancer. Our lab has been studying Musashi1 (Msi1), an RBP expressed in undifferentiated neural stem/precursor cells during both, embryonic an adult stages (Sakakibara et al. 1996). High levels of Msi1 have been reported in different tumors, including glioblastoma (GBM) (Ma et al. 2008). We are also interested in a small group of miRNAs that include miR-137, that induces neuronal differentiation of stem cells and inhibit proliferation of GBM cell lines (Santos et al. 2016). Vo et al. (2011) previously shown that Msi1 is regulated by several tumor suppressor miRNAs (Vo et al. 2011), and that they have opposite roles in neurogenesis and glioblastoma development. Here, we unveil a novel aspect of this antagonistic relationship. In the particular case of Msi1 and miR-137, our results prove that both share a large number of interconnected target genes implicated in functions critical to neurogenesis and glioblastoma growth. We put forward a model in which Msi1 and miR-137 regulate this network of targets in opposite directions (activation vs. repression) to contribute to cell fate decisions (self-renewal, differentiation, tumorigenesis) in glioblastoma.
Shaolei Lu
Warren Alpert Medical School of Brown University, USA
Title: GRP52 is a new sensitive markers for detecting metastatic prostatic carcinoma.

Biography:
Shaolei Lu has completed his Ph.D. at University of Massachusetts Amherst and his MD from Shanghai Medical College of Fudan University. He is currently a surgical pathologist at Brown University. He has published more than 35 peer-reviewed papers in reputed journals.
Abstract:
Metastatic prostate cancer is frequently presented as cancer of unknown origin. To confirm the prostatic origin, prostate-specific antigen (PSA), prostein, HoxB13, and NKX3.1 are frequently used. However, these markers are regulated by androgen receptor (AR) and their expression could be suppressed by hormonal therapy or altered by chemoradiation. Based on data mining of publicly available protein expression database and AR response gene database, we identified a new markers, GRP52, and compared it to the above markers in a series of metastatic prostate cancer.
We collected 46 metastatic prostate tumors, including 16 bone metastases (10 treated by hormonal ablation or chemoradiation and 6 untreated) and 30 non-bone metastases (27 treated vs 3 untreated). Immunostains of all the markers were performed and positive expression is defined as more than 5% of tumor cells with unequivocal staining in an appropriate pattern.
In 27 cases of treated non-bone metastasis, the positivity rates for GPR52, NKX3.1, HoxB13, and Prostein are 100%, 87.5%, 83%, and 67%, respectively. Out of 3 cases of untreated non-bone metastasis, GRP52 missed 1 and prostein missed 2, while NKX3.1 and HoxB13 detected all of them. For 9 cases that are negative for prostein, GPR52, NKX3.1, and HoxB13 could be detected in 4, 8,7, and 6 cases, respectively. All 5 markers were detected in all 16 bone metastases, except that HoxB13 could not be detected in 2 of 10 cases of treated bone metastasis.
Combination of multiple markers can increase the detection sensitivity for treated metastatic prostate cancer. Decalcification has less impact on the detection of major prostatic cancer marker.
M Ozge Tepe
Istanbul University, Turkey
Title: Histopathological findings in surgically resected treatment-resistant epilepsy cases

Biography:
M. Ozge Tepe graduated from Istanbul University, Istanbul Faculty of Medicine at the age of 24 years. Dr. Ozge Tepe has trained medical pathology during her residency since 2014.
Abstract:
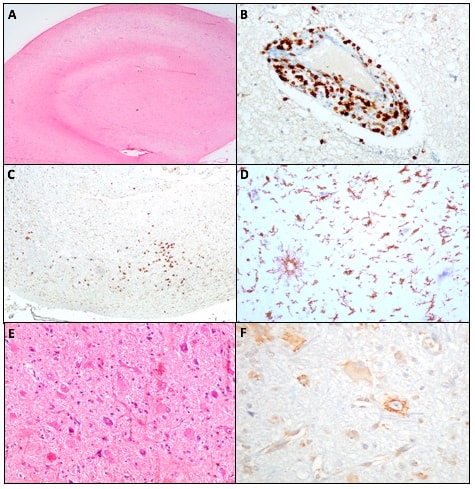
Statement of the Problem: In treatment-resistant epilepsy, different etiologies, histomorphological and immunohistochemical features, and diseases are included. Hippocampal sclerosis and focal cortical dysplasia are the most common histopathological diagnosis while tumor, vascular malformation, encephalitis, and glial scar are featured in decreasing frequency. Hippocampal sclerosis and focal cortical dysplasia are histopathologically classified according to the International League Against Epilepsy (ILAE) classifications. Molecular genetic studies in recent years have been effective in determining targeted therapies in patients who do not respond to antiepileptic drugs. mTOR pathway and immune system activation have been shown to play a role in epileptogenesis. To determine the incidence of different etiologies in the treatment-resistant epilepsy patients and find out histomorphological and immunohistochemical features and to demonstrate the relation between the ILAE subtypes and the clinical features and try to predict the prognosis of the patients were main purposes in a neuropathological examination of our surgically resected treatment-resistant epilepsy cases.
Methodology & Theoretical Orientation: In addition to immunohistochemistry (NeuN, Neurofilament-H, CD34, GFAP, IDH-1, and Olig-2) was performed in the diagnostic process, pS6 was used to demonstrate mTOR pathway activation in FCD cases and CD3, CD8, Iba-1 antibodies were applied to demonstrate neuroinflammation in HS cases.
Findings: Statistical analysis of HS and FCD, were the most frequent histological findings, revealed a significant difference in age of seizure onset, epileptic seizure duration, surgical age, gender status, and Engel classification. pS6 expression was observed in dysmorphic neurons and balloon cells in the cases of FCD type II while lymphocyte infiltration was seen in all HS cases.
Conclusion & Significance: Significant pS6 expression in FCD type II indicates that mTOR pathway inhibitors may be involved in the treatment of epilepsy. In HS cases, no statistical significant pathological feature to predict efficacy of immunomodulating therapy in a special subgroup has been identified.
Figure: (A) Hippocampal sclerosis showing neuronal loss in CA1 and CA4. (B) Perivascular CD3 immunopositivity. (C) Paranchymal CD3 immunopositivity. (D) Microglial cells showing Iba-1 immunopositivity. (E) Focal cortical dysplasia containing dysmorphic and balloon cells. (F) pS6 immunopositivity in dysmorphic cells and baloon cells.
Wenyi Luo
University of Texas MD Anderson Cancer Center, USA
Title: HuR (ELAV1) as a potential tumor marker in gastroesophageal junction (GEJ) adenocarcinoma

Biography:
Wenyi Luo has completed his MD from Peking University Health Science Center (China) and PhD from the University of Alabama at Birmingham. He also completed his combined anatomical and clinical pathology residency training from the University of oklahoma Health Sciences Center. He is currently a surgical pathology and gastrointestinal pathology fellow at MD Anderson Cancer Center. He has publised multiple papers in reputed journals.
Abstract:
HuR is a master protein involved in regulation of mRNA stability. Increased HuR expression and cytoplasmic translocation in tumors are associated with poor prognoses and altered responses to chemotherapy. HuR expression has been studied in esophageal squamous cell carcinoma, but not in GEJ adenocarcinoma arising in Barrett's esophagus. To study HuR, formalin fixed paraffin embedded tissue blocks of twenty patients who underwent endoscopic mucosal resection for GEJ adenocarcinoma without pre-operative neoadjuvant therapy and five patients with Barrett's esophagus without dysplasia were retrieved upon approval of Institutional Review Board. Tissue blocks were sectioned and stained with 1: 500 diluted mouse monoclonal anti-Human HuR antibody clone HuR-Rb SC-5261 (Santa Cruz, CA) and a horseradish peroxidase conjugated secondary antibody with a Leica BOND-III automated IHC / ISH-stainer. The cytoplasmic and nuclear staining patterns of HuR were evaluated separately and scored. The intensity and cytoplasmic localization of HuR staining correlate with neoplastic potential of the lesion. HuR staining is only detected in nuclei of benign metaplastic columnar mucosa (nuclear AIRS: 2.3; cytoplasmic AIRS: 0). Barrett’s epithelium shows stronger nuclear staining (AIRS: 6.0) and some cytoplasmic staining (AIRS: 5.2). Adenocarcinomas including poorly-differentiated adenocarcinoma and adenocarcinoma with mucinous differentiation show markedly increased HuR staining in both nuclei (AIRS: 9.4) and cytoplasm (AIRS: 9.4). In specimens with Barrett’s epithelium and dysplasia, HuR expression appears higher in the latter. This study provides a potential novel diagnostic and differential diagnostic marker of esophageal glandular neoplasms and may also provide a novel therapeutic opportunity.
Salha Sassi
The Ohio State University, USA
Title: Novel Slit/Robo and CXCL12/CXCR4-mediated signaling mechanisms that modulate small cell lung cancer progression and metastasis

Biography:
Abstract:
Small cell lung cancer (SCLC) represents 20% of lung cancers and is characterized by early dissemination, development of chemoresistance and a poor prognosis. Small cell lung cancer (SCLC) is a highly aggressive malignancy with a limited spectrum of therapeutic options. Therefore, identifying early biomarkers and targets may lead to the development of innovative therapies that will improve the survival of SCLC patients. Slit2, a secreted glycoprotein, has been shown to be suppressed in a number of cancers. Slit2 has recently emerged as an important tumor suppressor gene and acts through Roundabout Homolog1 (Robo1) receptor. Slit2/Robo1 signaling has been reported to inhibit the migration of a variety of cancer cells including non-small cell lung cancer (NSCLC). The chemokine receptor CXCR4 and its cognate chemotactic ligand CXCL12 play an important role in cell migration, cancer growth, angiogenesis, and metastasis. However, the molecular mechanism by which the Slit/Robo complex inhibits the migration of small cell lung cancer is not well defined. Aims: Determine Slit2and Robo1 expression in a wide range of pulmonary neuroendocrine carcinomas (NEC), including SCLC and in human SCLC patient samples 2. Analyze the role of Slit2 in tumor growth and metastasis in vivo using a Small cell lung cancer mouse model.3. Investigate the role of Slit2/Robo1 signaling pathway modulates the CXCL12/CXCR4-induced chemotaxis and metastasis in Small cell lung cancer.
Materials and Methods: Here, we evaluate the anti-cancer and anti-metastatic potential of Slit2 protein using mouse models. Cell lines, we used highly metastatic SBC5 and SBC3 small cell lung cancer cell lines. Slit2 and Robo1expression were analyzed by immunofluorescence, western blot and Fluorescence-activated cell sorting of live cells (FACS) by using anti-Slit2 (Abcam) and anti-Robo1 (Chemocentryx) antibodies. Further in vitro cell migration, invasion, and colony assays, Modified Boyden chambers (Coster) were coated with 0.1% gelatin (for migration assays) or extracellular matrix components (for invasion assays). Experimental Design: To evaluate the potential role of Ad-Slit2 in tumor growth and metastasis in small cell lung cancer in vivo. Animal studies, all animal work was done in accordance with protocols approved by the Institutional Animal Care and Use Committee at the Ohio State University. Female athymic nude mice, SBC5 cell lines were transduced with lentivirus-encoding luciferase were injected subcutaneous injection and through Tail –vein. Quantitative real-time PCR, The total RNA from either cell lines or tumor tissue was extracted using a QIAGEN RNeasy kit. Immunostaining, all staining was performed in formalin-fixed, paraffin embedded 8-mm-thick tumor. Slides were incubated with primary antibody for Ki67, Cytokeratin, and CD31.
Results: Slit2 regulates metastatic potential of small cell lung cancer cells in vitro. To understand the role of Slit in SCLC pathogenesis, we first assessed the expression of Robo1 and Slit2 in SBC5, a highly metastatic SCLC cell line, and SBC3, a low metastasizing SCLC cell line. By western blot analysis and immunofluorescence, we found that Slit2 expression was very low in SBC5 compared to SBC3 and normal epithelial cell line, BEAS. In addition, we showed that 90% of SBC5 showed expression for Robo1, while 39% cells showed expression in SBC3 by FACS Expression of typical SCLC markers Slit2, Robo1 of the SBC3 and SBC5 cell lines were tested in RT-qPCR relatively to RNA from normal lung cell line. Since Slit2 is a secretory protein, we demonstrated the presence of Slit2 in the conditioned media of SBC3 cells. Recombinant soluble Slit2 was shown to inhibit cell migration, invasion and wound healing in SBC5 and SBC3 cells. These effects were mediated through Robo1. Furthermore, we found CXCR4 expression was high in SBC5 compared to SBC3. Also, we found that soluble Slit2 treatment significantly reduced the number of tightly packed colonies in a colony formation assay using SBC5 cells, suggesting that Slit2 acts as a tumor suppressor in SCLC. In addition, we observed that Slit2 inhibited CXCL12-induced cell migration, chemoinvasion, and chemotaxis To further analyze the molecular mechanism of Slit2 -mediated signaling, we observed characterized Slit-2- mediated inhibition of the CXCL12/CXCR4 chemotactic pathway and found that Slit-2 can block the CXCL12- induced activation of the Src and PI3K kinases. In addition, Slit-2 inhibited the CXCL12- induced activation of MAPKs, it inhibited the Akt phosphorylation and Rac activation induced by this chemokine. Slit2 reduces small cell lung tumor growth and inhibits metastasis in vivo. To evaluate the potential role of Ad-Slit2 in the development of tumor and metastasis in mice model. We first established a mouse model of small cell lung cancer. Then, we injected luciferase-labeled SBC5 SCLC subcutaneous injection and Tail-vein and after confirmed of tumor establishment with bioluminescence imaging, mice were treated control group (Ad-Null) and another group (Ad- Slit2) treatment twice weekly. Both groups underwent weekly bioluminescence imaging to monitor tumor growth. All mice were subsequently sacrificed and their tumors collected and analyzed. Compared with the Ad-Null group, Ad-Slit2 mice had significantly lower tumor burden in 1/6 than controls 6/6. Using a syngeneic mouse model, we reported that the ectopic expression of Slit2 using Adeno-Slit2 transduction successfully restrains tumor growth and also significantly inhibited liver, bone, and brain metastasis compared to the Adeno-null control group. Subsequently, Immunohistochemistry of Ki67 and CD31 depicted that Slit2 decreases angiogenesis and proliferation. It is thus curious that Slits found to function as a chemoattractant for vascular endothelial cells.
Conclusion, these studies reveal that Slit2 and Robo1 may play an important role in small cell lung tumor progression and metastasis and could be used for the development of novel and targeted therapies for highly aggressive small cell lung cancer

Biography:
Mansoureh Haghighi has completed her Ph.D. at the age of 39 years from Isfahan University of Medical Sciences . she is the director of HLA banking of MAHAK hospital, a children's cancer pediatric hospital. she has published this paper in molecules journal.
Abstract:
The B-lymphocyte antigen CD20 (CD20) is a target of active agents in the diagnostic and 12 treatment of all types of B-cell lymphomas and leukemia. The extracellular domain loops of the 13 CD20 protein could be suitable targets for single-stranded nucleic acid oligomer (aptamers). 14 a(ssDNA) aptamers binding CD20, and to characterize their potency. CD20 was expressed in the 15 human embryonic kidney cells (HEK293T) and ssDNA library containing 52 randomized 16 nucleotides (nt) flanked by two 18-nt primers sites was constructed. Elevenrounds of Cell-SELEX 17 were performed and the selected ssDNA pool was amplified by polymerase chain reaction(PCR), 18 ligated with pTZ57T/A –pcDAS3.1 Hygro(+) vector and used to transform competent Escherichia 19 coli TOP10 cells. The plasmid o resulted clones were extracted and sequenced by M13 forward 20 primers. The results of sequencing revealed 10 different aptamers that shared some common 21 conserved regions. The secondary structures of the aptamers were predicted using the DNAMAN 22 software and three aptamers with the highest thermodynamic stability were selected (AP-1 to 23 AP-3). AP-1 aptamer was the most thermodynamically stable (ΔGAP-1 = -10.87 kcal/mol) with a 24 highest binding affinity (96.91 ± 4.5 nM) to the membranous CD20 protein. Further studies demand 25 to develop methods to use these apatmaers for diagnostic and therapeutic purposes in 26 CD20-related diseases.

Biography:
Clinical Project Manager at Cedars-Sinai, USA
Abstract:
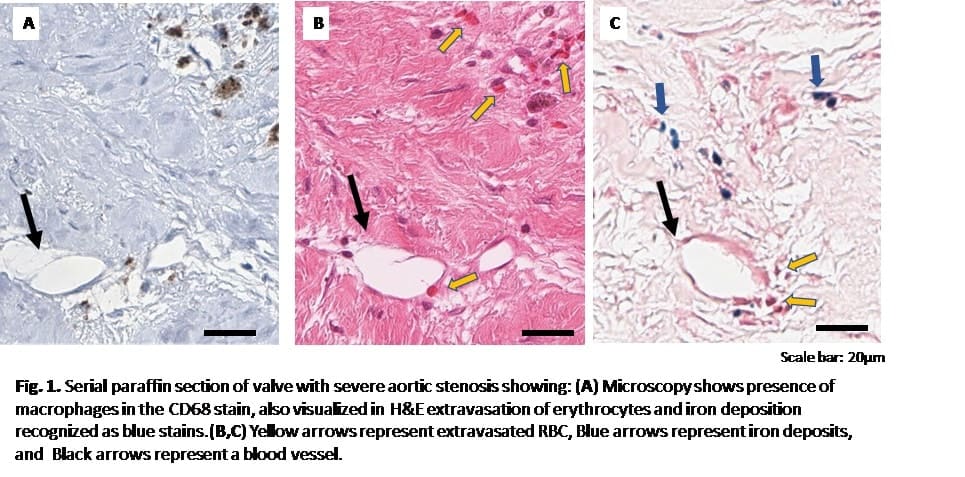
Introduction: Calcific aortic stenosis (AS) is characterized by calcification, restricted leaflet motion and reduction in valve area. It has been shown that neovessels, intraleaflet hemorrhage and iron deposition may be involved in the pathophysiology of the disease. We sought to evaluate the association between aortic valve intraleaflet neovascularization and iron deposition in patients with AS using histologic techniques.
Methods: Aortic valve leaflets of 10 consenting patients with AS were extracted during surgical aortic valve replacement, fixed, embedded and sectioned. Presence of microvessels, macrophages, and iron were assessed with standard immunohistochemical staining with CD34, CD68 and iron respectively. Histological analysis was performed using Leica software. For each stain, the areas of CD34, CD68, and iron positive pixels were calculated. To assess linear dependence between variables, the Pearson's correlation coefficient for normally distributed or Spearman's rank correlation coefficient for non-normally distributed variables was calculated. A value of p < 0.05 was considered statistically significant.
Results: The demographic characteristics, risk factors, and echocardiography of study patients are summarized in Table 1. There was a positive correlation between detection of cd34 cells and iron (r = 0.7, P = 0.02). Detection of CD34 cells was also positively correlated with the peak transvalvular gradient (0.41, p = 0.5), and negatively associated with valve area (r = -0.14, p=0.05).
Conclusion: Our results suggest that iron deposition occurs in association with neovascularization. These preliminary findings support the hypothesis that angiogenesis may promote intraleaflet inflammation by allowing iron deposition.
Table 1
|
Patient Characteristics |
(n= 11) |
|
|
Male, n (%) |
8 (72) |
|
|
Age (years) mean ± SD |
66.5 ± 3 |
|
|
Risk Factors |
|
|
|
Hypertension, n (%) |
8 (72) |
|
|
Diabetes mellitus, n (%) |
0 (0) |
|
|
Hyperlipidemia, n (%) |
9 (81) |
|
|
Smoking, n (%) |
5 (45) |
|
|
Anticoagulants, n (%) |
5 (45) |
|
|
Echocardiography |
|
|
|
Peak gradient (mmHg) |
60.8 ± 6 |
|
|
Mean gradient (mmHg) |
36.7 ± 4 |
|
|
LVEF (%) mean |
64.7 ± 0.01 |
|
|
AVA (cm2) |
0.94 ± 0.15 |
|
|
|
|
|
Daniela Tosoni
European Institute of Oncology, Italy.
Title: Loss of Numb in breast carcinogenesis: a paradigm for a mechanism-based selective anti-cancer stem cell therapy

Biography:
Daniela Tosoni has completed her PhD from The European Institute of Oncology and Yale University and postdoctoral studies from The European Institute of Oncology and The FIRC Institute for Molecular Oncology in Milan. She is a Staff Scientistic and the Coordinator of Stem Cell and Preclinical Model Unit of the Program of Molecular Medicine at European Institute of Oncology.
Abstract:
The cell fate determinant Numb is a tumor suppressor in the mammary gland whose loss in human breast cancers results in p53 inactivation and an aggressive disease course. Numb-p53 downregulation leads to aberrant mammary morphogenesis and emergence of cancer stem cells (CSCs). Numb-deficient CSCs show unlimited self-renewal and proliferative potential, which is a function of their ability to execute unchecked self-renewing symmetric divisions. These phenotypes that can be reverted by Numb-p53 restoration in a Numb-knockout mouse model, arguing that targeting Numb-p53 dysfunction in Numb-deficient human breast cancer could represent a novel anti-CSC therapy. Using patient-derived xenografts, we have recently demonstrated that expansion of the CSC pool, due to altered self-renewing divisions, is also a distinguishing feature of naturally occurring Numb-deficient human breast cancers. In these cancers, using the inhibitor Nutlin-3 to restore p53, we corrected the defective self-renewal properties of Numb-deficient CSCs and inhibited CSC expansion, thus curbing tumorigenicity and metastasis. Remarkably, a regimen combining Nutlin-3 and chemotherapy induced persistent tumor growth inhibition, or even regression, and prevented CSC-driven tumor relapse after removal of chemotherapy. We therefore provided a pre-clinical proof-of-concept that targeting Numb-p53 dysfunction results in a specific anti-CSC therapy in Numb-deficient human breast cancers. We will discuss the value of the CSC paradigm to address breast cancer heterogeneity and how functional assays based on the biology of CSCs should complement the currently used RECIST criteria for the evaluation of the efficacy of novel anti-cancer therapeutics, in the ultimate perspective of developing effective mechanism-based therapies to eradicate breast cancer.
Brian Lifschutz
Des Moines University College of Osteopathic Medicine, USA
Title: The role of IL-38 in the growth of bladder cancer: Evidence as a cancer growth inhibitor

Biography:
Brian Lifschutz has completed his BS in Biology from the Pennsylvania State University and is currently a second-year Osteopathic medical student at Des Moines University. During his undergraduate career, he has worked with the model organism Drosophila melanogaster to characterize genetic changes that contribute to neurodevelopmental disorders such as autism, intellectual disability, and schizophrenia.
Abstract:
Background: Bladder cancer (BC) is the second leading cancer of the genitourinary system. About 81,190 new cases of bladder cancer are projected to occur in the United States in 2018. Interleukin-38 (IL-38) is a newly found cytokine belonging to the IL-1 family of cytokines and nothing is known about its role in the pathogenesis of neoplasia. This study was designed to investigate the direct role of IL-38 on the growth of BC.
Methods: Clonogenic survival assay, cell proliferation, and caspase-3 activity kits were used to evaluate the direct effects of IL-38 on cell survival, proliferation, and apoptosis of the widely studied bladder cancer cell line T24. We further investigated possible molecular mechanisms using RT-PCR and immunocytochemistry.
Results: The percentage of colonies of T24 BC cells decreased significantly in the presence of IL-38. This was paralleled by the decrease in the OD value of cancer cells in the presence of IL-38. Furthermore, the relative caspase-3 activity in cancer cells increased significantly in the presence of IL-38. The anti-tumor effect of IL-38 on T24 BC cells correlated with decreased pro-proliferative molecule CDK4. The pro-apoptotic effect of IL-38 correlated with decreased anti-apoptotic molecules Bcl-2 and survivin.
Conclusions: IL-38 might be a growth inhibitor of BC through the inhibition of proliferation and promotion of apoptosis via the modulation of CDK4, Bcl-2, and survivin. Such a study might be helpful to develop immunotherapy for BC.
Saran lotfollahzadeh
Shahid Beheshti University of Medical Sciences,Iran
Title: Surgical outcomes in patients with disorders of sex development in Mofid Children’s Hospital, 2001-2014

Biography:
Saran lotfollahzadeh has completed her MD at the age of 25years from Markazi University of Medical Sciences,Iran. She continued her General Surgery residency during 2010 to 2015 at Shahid Beheshti University of Medical Sciences. Following that she started her Pediatric Surgery fellowship from 2016 at Mofid Children’s Hospital. She has published more than 19 papers and is an instructor of General surgery. She has published 36 books in the field of General Surgery and pediatric Subspecialty.
Abstract:
Disorders of Sex Development is a childhood and infantile anomaly that affect not only the somatic growth; but also leading to stress and anxiety among parents who are seeking optimal treatments. Accordingly in this study the surgical outcomes in patients with Disorders of Sex Development in Mofid Children’s Hospital from 2001 to 2014 were determined.
In this case series study 72 consecutive children with Disorders of Sex Development in Mofid Children’s Hospital from 2001 to 2014 were enrolled and followed in a regular manner. Data were gathered by existing medical documents and were recorded in prepared checklist. The surgical outcomes were assessed with interview and clinical examination after announcement by hospital. The success and complication rate were determined by group of surgeons and compared according to other variables. In the current study we have evaluated seventy two patients; 55 (76.38%) affected by Congenital Adrenal Hyperplasia, thirteen (18.05%) by Testicular Feminization , 2 (2.7%) by OvoTesticular Disorder and two case (2.7%) by Mixed Gonadal Dysgenesis (MGD). Most common type of applied surgery was Clitroplasty, Genitoplasty and Pullthrough Vaginoplasty (table1). Fifty nine patients (81.9%) had no surgical complications. All patients had good conditions at discharge and no mortality was registered. Three cases of Testicular Feminization (4.2%) Who Underwent pulltrough colovaginoplasty were married. According to our findings, surgical outcomes in cases of Disorders of Sex Development are relatively good and satisfactory. However long-term follow-up study is required to determine the final outcomes especially for marital and sexual issues.
Table 1- Surgical Techniques
|
MGD |
Ovotesticular |
Testicular Feminization |
CAH |
Valid Percent |
Frequency |
Type of surgery |
|
1 |
1 |
- |
45 |
65.3 |
47 |
1- Clitoro plasty + Vaginoplasty + Genitoplasty |
|
- |
- |
- |
9 |
12.5 |
9 |
2-Clitoroplasty + Genitoplasty + colovaginoplasty |
|
_ |
_ |
_ |
1 |
1.4 |
1 |
3- Urethroplasty + Scrotoplasty + hysterectomy + bilateral salpingo-oophorectomy |
|
_ |
1 |
- |
- |
1.4 |
1 |
4- Hysterosalpangectomy + Left Gonadectomy + Right Orchidopexy |
|
1 |
- |
- |
_ |
1.4 |
1 |
5-Genitoplasty + ColoVaginoplasty + Left Orchidectomy |
|
_ |
_ |
13 |
_ |
18.1 |
13 |
6- ColoVaginoplasty + Bilateral Gonadectomy |
|
2 |
2 |
13 |
55 |
100 |
72 |
Total |
Wasswa William
Mbarara University of Science and Technology, Uganda
Title: Automated segmentation of the nucleus, cytoplasm, and background of pap-smear images using a Trainable Pixel Level Classifier

Biography:
Wasswa William is a Ph.D. Student (Biomedical Engineering) at Mbarara University of Science and Technology, Uganda. He has a masters in Biomedical Engineering from the University of Cape Town, South Africa. He has valuable experience in the fields of Medical Devices, Medical Imaging, and Machine Learning.
Abstract:
Background: Cervical cancer ranks as the fourth most prevalent cancer affecting women worldwide and its early detection provides the opportunity to help save a life. Automated diagnosis and classification of cervical cancer from pap-smear images has become a necessity as it enables accurate, reliable and timely analysis of the condition’s progress. Segmentation is a fundamental aspect in enabling successful automated pap-smear image analysis. In this paper, a potent algorithm for segmentation of the pap-smear image into the nucleus, cytoplasm, and background using pixel level information is proposed.
Methods: First, a number of pixels from the nuclei, cytoplasm, and background are extracted from five hundred images. Second, the selected pixels are trained using noise reduction, edge detection, and texture filters to produce a pixel level classifier. Third, the pixel level classifier is validated using the test set and 5- fold cross validation using Fast Random Forest, Naïve Bayes, and J48 classification techniques.
Results: An extensive evaluation of the algorithm and comparison with the benchmark ground truth measurements shows promising results. Comparison of the segmented images’ nucleus and cytoplasm parameters (nucleus area, longest diameter, roundness, perimeter and cytoplasm area, longest diameter, roundness, perimeter) with the ground truth segmented image feature parameters (nucleus area, longest diameter, roundness, perimeter and cytoplasm area, longest diameter, roundness, perimeter) yielded average errors of 0.94, 0.93, 0.02, 0.63, 0.96, 0.37, 0.13 and 0.96 mm respectively. Validation of the proposed pixel level classifier with 5-fold cross-validation yielded a classification accuracy of 98.48%, 94.25% and 98.45% using Fast Random Forest, Naïve Bayes, and J48 classification methods respectively. Finally, validation with a test dataset yielded a classification accuracy of 98.48% and 98.98% using Fast Random Forest and J48 Classification methods respectively.
Conclusions: This paper articulates a potent approach to the segmentation of cervical cells into the nucleus, cytoplasm, and background using pixel level information. The experimental results show that the approach gives good classification and achieves a pixel classification average accuracy of 98%. The method serves as a basis for first level segmentation of pap-smear images for diagnosis and classification of cervical cancer from pap-smear images using nucleus and cytoplasm pixel level information.
Mehwish Gilani
Armed Forces Insttitute of Pathology, Pakistan
Title: Spectrum of renin angiotensin aldosterone system disorders in young hypertensives of pakistan

Biography:
I completed my MBBS from Army Medical college Rawalpindi (National University of Sciences & Technology) in 2009. Currently Iam undergoing my FCPS part II training in Chemical Pathology in Armed Forces Institute of Pathology,Rawalpindi.I am actively involved in Reasearch projects and two more projects are in the pipeline.
Abstract:
The study was a cross sectional study conducted at the Department of Chemical Pathology & Endocrinology Armed Forces Institute of Pathology (AFIP) Rawalpindi from Jan 2016 to Dec 2016. One hundred and sixty-five young hypertensive subjects, aged 17-40 years, of either gender presenting in the outpatient department (OPD) were recruited from local population of Rawalpindi. All subjects were having blood pressure more than 140/90 mm of Hg and were not on any anti-hypertensive medicine. Patients with renal dysfunction, heart failure, pregnancy and secondary hypertension were excluded from the study. Blood sample was taken from each patient to analyze arterial blood gases, plasma renin, serum aldosterone and electrolytes. Sandwich chemiluminescence immunoassay and ELISA techniques were used to analyze plasma renin and serum aldosterone level. Arterial blood gases and electrolytes like sodium and potassium were measured by potentiometry, while bicarbonate was calculated. Normally distributed continuous variables were presented as mean+SD and others as median. Multiple regression analysis was performed to compute association of age, electrolytes, systolic and diastolic blood pressure in OPD and Endocrine Clinic AFIP with Essential hypertension and Primary hyperaldosteronism. P<0.05 was considered statistically significant. Out of 80 subjects, 72 were diagnosed with Essential hypertension and 08 with Primary hyperaldosteronism. None of the patients had Liddle syndrome, apparent mineralocorticoid excess or Gordon syndrome. Mean age of patients having Essential hypertension was 30.97+7.13 years, whereas those with Primary hyperaldosteronism was 29.25 + 7.1 years. Mean serum sodium was 137.8 + 6.5 mmol/l and potassium was 4.23 + 0.6 mmol/l. Mean systolic blood pressure of patients measured in OPD was 172.7+19.2 mm of Hg whereas diastolic blood pressure was 100.0+8.3 mm of Hg. Mean systolic blood pressure measured in Endocrine Clinic AFIP was 142.7 + 10.5 mm of Hg and diastolic blood pressure was 90.3+6.5 mm of Hg. Diastolic blood pressure was significantly higher (p = 0.001) among all the patients reported in OPD. No statistically significant association was found between age, systolic and diastolic blood pressure (p < 0.05) in either OPD or Endocrine Clinicic.Therefore, it was concluded that hypertension is not uncommon in young population of Pakistan. Primary hyperaldosteronism as compared to other RAAS disorders, remains the leading cause of hypertension in young population.
Nelson Sham
Des Moines University College of Osteopathic Medicine, USA
Title: Raspberry: A fighter against cervical cancer

Biography:
Nelson Sham has completed his BS in Cellular and Developmental Biology at the age of 22 years from University of California, Santa Barbara. He is currently a second-year Osteopathic medical student at Des Moines University.
Abstract:
Background: Cervical cancer (CC) is one of the leading causes of death among women worldwide. We have previously reported that blueberry extract constrains the growth of CC. Raspberry is a widely consumed fruit and its anti-tumor activity has been shown in some cancers. However, little is known about its direct effect on CC. This study was designed to investigate the direct role of raspberry in the growth of CC and its potential mechanisms.
Methods: Clonogenic survival assay, immunocytochemistry (ICC), TUNEL staining and caspase-3 activity kit were used to evaluate the effects of raspberry extract (RE) on cell survival, proliferation, and apoptosis of a widely-used CC cell line, HeLa. We further investigated the possible molecular mechanisms by using RT-PCR and ICC.
Results: We found that the percentage of colonies and PCNA staining intensity of HeLa cells decreased in the present of RE. TUNEL+ cells and the relative caspase-3 activity in cancer cells increased in the presence of RE. The anti-proliferative effect of RE on HeLa cells correlated with the increased expression of anti-proliferative molecule p53 and the increased expression of pro-apoptotic molecule Fas.
Conclusions: RE notably constrains the growth of CC by inhibiting its proliferation and promoting its apoptosis, suggesting the anti-tumor property of RE in CC.
Zeinab Ghasemishahrestani
Federal University of Rio de Janeiro, Brazil
Title: Evaluation of the antitumoral effects and mechanisms of action of novel binuclear cu-complexes on tumorigenesis.

Biography:
Zeinab Ghasemishahrestani has completed her MSc in Biochemistry from Pune University in India with O grade and she is doing the Ph.D. in UFRJ in Brazil regarding cancer research under guidnce of professors Marcos Dias Pereira and Andre Luis Souza dos Santos. she is publishing 5 papers in reputed journals.
Abstract:
Cancer is one of the major causes of death across the world. Hence, development of chemotherapeutic strategies involving novel antitumor agents has been the focus area of cancer treatment. The anticancer activities of copper complexes have been the focus of much research to discover novel anticancer agents. Current study deals with the effects of two novel binuclear copper (II) complexes with N2O-doner tridentate ligands (R9 and R10) on cytotoxic effects on breast (MCF-7), lung (A549) and prostate (PC3) cancer cell lines. MCF-7, A549 and PC3 cell lines were analyzed using MTT assay and Flow Cytometry intracellular ROS production assay. MCF-7, A549 and PC3 treated with R9 showed an IC50 of 1.282 ± 0.14, 1.428 ± 0.07 and 1.60± 0.08, respectively. On the other hand, MCF-7, A549 and PC3 cell lines affected by R10 exhibited (IC50 =1.006 ± 0.18, IC50=1.138 ±0.22, IC50=1.44± 0.12, respectively). Flow cytometry assay for MCF-7 and A549 at three different concentrations 0.5, 1 and 2 μM illustrated that cells tested with R9 and R10 presented ROS accumulation in a dose-dependent manner. In case of testing some of R9 and R10 concentration, the increase of ROS production was even higher than the positive control, doxorubicin. Cytotoxicity and induction of high amount of ROS may considered R9 and R10 a potential therapeutic agent for breast, lung and prostate cancer. We will further work on these compounds to understand the exact mechanism of action of these novel complexes to pursue our investigation on their effects in vitro and in vivo.
Mikayla M Brockmeyer
Des Moines University College of Osteopathic Medicine, USA
Title: Grapefruit as a possible radiosensitizer for prostate cancer

Biography:
Mikayla is working on her MS in Biomedical Sciences from Des Moines University. She is a graduate student researcher working in the Fang lab and hopes to attend medical school in the future.
Abstract:
Background: Prostate adenocarcinoma is the most common cancer diagnosis excluding melanoma in men living in the US Grapefruit extract contains active compounds known to have antioxidant, anti-inflammatory, and potentially anticancer properties. Previously, our lab has published research on proposed molecular mechanisms of resveratrol and IL-37 as phytochemical and cytokine radiosensitizers of prostate cancer, respectively; however, there are no data on the anticancer effects of grapefruit extract on prostate cancer to date. The aim of this study was to evaluate the effect of grapefruit extract and radiotherapy on the cell proliferation, survival, and cell death, using the PC-3 prostate cancer cell line.
Material and Methods: Clonogenic assay, PCNA staining, Quick Cell Proliferation assay, TUNEL staining, and caspase-3 activity assay was used to investigate the role of grapefruit extract in human prostate cancer growth, survival, and cell death. PC-3, a widely characterized cell line, was used in these experiments. We further investigated the possible molecular mechanisms using RT-PCR and immunohistochemical staining.
Results: Exogenous administration of grapefruit extract in combination with radiation treatment resulted in a decrease in the percentage of colonies of PC-3 cells. This finding correlated with the increased measurement of caspase-3 activity by a caspaseâ€3/CPP32 colorimetric assay kit. The anti-proliferative effect of GE and RT is currently under investigation, in addition to the increase in pro-apoptotic effect in PC-3 cells.
Conclusion: These results suggest a role for exogenous grapefruit extract as a radiosensitizer for prostate cancer, which may lead to a promising new avenue for enhancing current therapeutic options.
Anuradha Garg
Post Graduate Institute of Medical Education & Research (PGIMER), India
Title: APOBEC3G governs cellular oncogenic transformation

Biography:
A native of India, Anuradha Garg received her B.Sc. (Biotechnology, Biochemistry and Genetics) from Bangalore University (India) and M.Sc. (Stem Cell & Tissue Engineering) from Panjab University (India). She completed her Ph.D. program at Postgraduate Institute of Medical Education & Research (PGIMER) at Chandigarh (India) in 2017. Her research goals are to gain insight into the role of APOBEC3G in controlling mRNA fate and to elucidate its function in tumorigenesis and immunesurveillance. She has published 5 papers in reputed International journals during here Ph.D.
Abstract:
The oncogenic potential of APOBEC3G gene was recently appreciated by its inhibitory influence of APOBEC3G upon miRNA-mediated repression of the gene responsible for hepatic metastasis. The present study employed human PBMCs, as an archetype model to understand the role of APOBEC3G in regulation of gene involved in oncogenesis. Such a study revealed that APOBEC3G transrepresses KLF4 by binding to its mRNA at 3’UTR. This phenomenon was paralleled by the sustained expression of the cellular SP1 that ensured overexpression of genes coding for c-myc, Bmi-1, BCL-2 and MDM2 coupled with downregulation of p53 in PBMCs thereby creating a favorable situation for oncogenic transformation. Additionally, cell cycle regulators like Cyclin D, B and E were found to be upregulated, along with increase in S-phase of the cell cycle. Furthermore, study revealed role of APOBEC3G in tailoring immune response that could help tumor growth through escape of immunosurveillance. This study unambiguously revealed that APOBEC3G has the inherent capacity to upregulate genes coding for STAT3, CCL5, IL-6, IL-4, and NF-κB coupled with downregulation of IL-10, IL-17. Based upon these results, we propose that increased expression of APOBEC3G could have the inherent capacity to ensure alterations of gene expression in such a way that leads to cellular proliferation, hallmark of oncogenesis as well as make the environment conducive for tumor progression and immune escape through its ability to ensure sustained chronic inflammation. This may add a new dimension to understand oncogenesis in general, and the novel role of APOBEC3G in the oncogenic process in particular.
Sourav Taru Saha
University of the Witwatersrand, South Africa
Title: Delving KS-01 as a novel therapeutic strategy in treating breast cancer

Biography:
Mr. Sourav Taru Saha is a PhD. student working on Breast cancer at the University of the Witwatersrand. The research group’s main focus is the link between Cholesterol and Breast cancer. Till now, his research has shown promising results and in 2018 the concept would be tested in vivo. Based on the results, this research might lead to a novel drug in treating Breast cancer.
Abstract:
Cancer cells have an increased need for cholesterol, which is required for cell membrane integrity. Cholesterol accumulation has been described in various malignancies including breast cancer. Cholesterol has also been known to be the precursor of estrogen and vitamin D, both of which play a key role in the histology of breast cancer. Thus, depleting the cholesterol levels in cancer cells is a proposed innovative strategy to treat cancer. Therefore, novel cholesterol-depleting compounds are currently being investigated. KS-01 is a cyclic amylose oligomer composed of glucose units. It solubilizes the cholesterol and is proven to be toxicologically benign in humans. This led us to hypothesize that it might deplete cholesterol from cancer cells and may prove to be a clinically useful compound. Our work provides preliminary experimental evidences to support this hypothesis. We identified the potency of KS-01 in vitro against two breast cancer cell lines: MCF-7 (Estrogen positive, ER+), MDA-MB-231(Estrogen negative, ER-) and compared the results against two normal cell lines: MRC-5 (Normal Human Lung Fibroblasts) and HEK-293 (Normal human embryonic kidney cells) using cytotoxic, apoptosis and cholesterol based assays. KS-01 treatment reduced intracellular cholesterol resulting in significant breast cancer cell growth inhibition through apoptosis. The results hold true for both ER+ and ER-. These data suggest that KS-01 can prevent cholesterol accumulation in breast cancer cells and is a promising new anticancer agent.
Angel Casacó Parada
Center for Molecular Immunology, Cuba
Title: The 14F7 monoclonal antibody: past, present and future for theragnosis in cancer

Biography:
Dr. Angel Casacó is graduaded of medicine at the Havana University School of Medicine in 1974 and completed his PhD at the age of 30 years from the Polish Academic of Science in Varsow, Poland. He has published more than 80 articles in important journals and some books and belong to many nacional and international Scientific Socities.
Abstract:
The relevance of certain gangliosides in tumor growth and metastatic dissemination has been well documented. GM3 (NeuGc) ganglioside is particularly interesting due to its restrictive expression in normal human and chicken tissues. On the other hand, previous studies have shown that 14F7 Mab (IgG1) is a very specific anti-NeuGcGM3 ganglioside inducing cell death accompanied by cellular swelling, membrane lesion formation, and cytoskeleton activation, suggesting an oncosis-like novel phenomenon. The fact that the 14F7 Mab is able to very specific recognize in-vitro and in-vivo by IHC and immunogammagraphyc studies the P3X63 murine myeloma cell line, the spontaneous epithelial chicken ovarian cancer and the human breast cancer that over-express the GM3 (NeuGc) ganglioside makes this Mab an important tool with anti-proliferative anti-tumor effects in vitro and in vivo animal models. A dose-escalation Phase I clinical trial is ongoing in Cuba with the humanized 14F7 Mab for studying the pharmacokinetic, toxicity and any evidence of anti-tumor effect in solid tumors over-expressing the GM3 (NeuGc). These two properties, the very specificity for recognizing tumors that over-express this ganglioside and its capability to have anti-tumor effect make this Mab an ideal drug for personalized medicine and teragnosis of cancer patients over-expressing the GM3 (NeuGc) ganglioside
Saran lotfollahzadeh
Shahid Beheshti University of Medical Sciences, Iran
Title: Two cases of cervical pediatric lipoblastoma

Biography:
Saran lotfollahzadeh has completed her MD at the age of 25years from Markazi University of Medical Sciences,Iran.She continued her General Surgery residency during 2010to 2015 at Shahid Beheshti University of Medical Sciences. Following that she started her Pediatric Surgery fellowship from 2016 at Mofid Children’s Hospital.She has published more than 19 papers and is an instructor of General surgery.She has published 36 books in the field of General Surgery and pediatric Subspecialty.
Abstract:
Lipoblastoma is an extremely rare entity, characterizing by benign nature, encapsulated tumor which most commonly diagnosed in upper and lower extremities and occasionally in the trunk. Cervical lipoblastoma is reported for approximately 50 cases worldwide.
Patients and method:
Case1: A 9 months old patient referred to our hospital with uni-lateral progressively enlarged neck mass for a couple of months before admission. On physical examination, painless movable four in three centimeters mass was revealed. Further imaging by CT elucidated a heterogeneous mass with spinal cord involvement.
Case2: A 2-year-old male patient who presented with a recurrent well-defined left sided submandibular mass for several months before admission without significant skin changes.
Results: Both patients underwent radical surgical excision for the neck mass. Local invasion to the adjacent vascular structures were not clarified. Gross pathological appearance revealed well-circumscribed mass which were differentiated from surrounding structures by connective tissue. Post operative course passed uneventfully.
Conclusions: Lipoblastoma as an uncommon clinical entity of cervical lesions might present as non-tender, uni-lateral neck mass. Radical surgical excision if possible without sacrificing vascular structures serves as the optimal modality of treatment and definitive diagnosis demand pathological evaluation.
Mahshid Jafari
Azad University of Science and Research, Tehran, Iran
Title: Co delivery of anti-cancer drugs by combination therapy

Biography:
Mahshid Jafari has completed his B.Sc. from Azad University of Tehran- North in Chemical Engineering and is a Master student in the same field and her thesis is about the Nano-medicine in cancer this Abstract is part of her thesis.
Abstract:
Among many cancer therapy, chemotherapy and photodynamic therapy (PDT) have been considered in this essay. For the enhancement of the drug delivery, the use of up-conversion material is taken into account. Under near-infrared (NIR) excitation, up-conversion emit ultraviolet light. in the traditional PDT, injecting the photosensitizer(PS), as a drug, then using illumination source like laser, light emitting diodes, arcing lamps and laser in order to active PS. Using up-conversion can help the drug to penetrate in more depth of the tumor tissue, compared to the traditional PDT, and improve the efficiency of the drug and finally the cancerous cell death. Additionally, we could assemble a core-shell nanoparticle to improve the chemotherapy as well as PDT. In regard to this, we could conjugated doxorubicin (DOX) in shell and then (PS) in core in order to deliver two anti-cancer. Then, the nanoparticle is PEGylated to overcome the dilemma of “protein corona”. Also, using Folic Acid (FA) for the cancerous cell receptor, as a ligand, in the endocytosis-mediated process, we could guarantee the targeted therapy.
Mohammad Ali Eghbal
Tabriz University of Medical Sciences, Iran
Title: Novel angiotensin receptor blocker, azilsartan induces oxidative stress and NFkB-mediated apoptosis in hepatocellular carcinoma cell line HepG2

Biography:
Mohammad Ali Eghbal has completed his PhD from University of Toronto in 2004. He is Professor of Pharmacotoxicology at Tabriz University of Medical Sciences, Tabriz, Iran. He has published more than 40 papers in reputed journals.
Abstract:
Over expression of renin angiotensin system (RAS) and nuclear factor-kappaB (NF-kB) has a key role in various cancers. Blockade of RAS and NF-kB pathway has been suggested to reduce cancer cell proliferation. This study aimed to investigate the role of angiotensin II and NF-kB pathway in liver hepatocellular carcinoma cell line (HepG2) proliferation by using azilsartan (as a novel Ag II antagonist) and Bay11-7082 (as NF-kB inhibitor). HepG2 cells were treated with different concentrations of azilsartan and Bay11-7082. Cytotoxicity was determined after 24, 48, and 72 h by MTT assay. Reactive oxygen spices (ROS) generation and cytochrome c release were measured following azilsartan and Bay11- 7082 treatment. Apoptosis was analyzed qualitatively by DAPI staining and quantitatively through flow cytometry methodologies and Bax and Bcl-2 mRNA and protein levels were assessed by real time PCR and ELISA methods, respectively. The cytotoxic effects of different concentration of azilsartan and Bay11- 7082 on HepG2 cells were observed as a reduction in cell viability, ROS formation, cytochrome c release and apoptosis induction. These effects were found to correlate with a shift in Bax level and a downward trend in the expression of Bcl-2. These findings suggest that azilsartan and Bay11- 7082 in combination or alone have strong potential for development as an agent for prevention against liver cancer after further studies.
Prakash Kinthada
JNTU University, India.
Title: Transition metal complexes/organometallic compounds as anticancer/anti HIV drugs or in pharmaceutical industry

Biography:
Prakash Kinthada is a Professor in Chemistry at Sri Vidyanikethan Engineering college, JNTU University in Ananthapur, A. Rangam Peta, Tirupathi, India.
Abstract:
Cancer is a dreadful disease and any practical solution in combating this disease is of paramount importance to public health. Cancer patients have burdened by drug induced toxic side effects, and no turned to seek help from the complementary and alternative medicine hoping for a better cure. Research on Platinum based drugs and Non Platinum based drugs is a Multi-Million Dollar Industry in USA and there is every need to produce safe drugs for the cure of this monstrous disease. Flavonoids have a long history of use in traditional medicines in many cultures. The phytochemical, curcumin is one of the major dietary flavonoid, belonging to a group of flavonol, Curcumin is a natural polyphenol. It is highly potential molecule capable of preventing and treating various cancers. Various dietary chemo preventive agents, turmeric powder or its extract are broadly used as therapeutic preparations in Indian System of medicine. We provide a summarized synthesis and structural determination of Curcumin Oxime, Curcumin Thiosemicarbazone derivative of Gold (III) complex. The use of these analogs for prevention of cancer tumor progression and treatments of human malignancies. A pharmacologic agent for treating and/or preventing cancer, among other diseases and conditions, and particularly breast, prostate, and pancreatic cancer, in humans and animals. The novel pharmacologic agent is an isoflavonoid or isoflavonoid mimetic covalently attached to a cytotoxic pharmacophore that, preferably has the ability to conjugate with a metal salt to form a more potent metal complex, particularly a Au (III) complex and other complexes of Platinum, Palladium, Ruthenium, Copper etc.
Fekadu Alemu
University of Science and Technology, Norway
Title: Expression and regulation of FSTL5 in multiple myeloma cells

Biography:
Fekadu Alemu Atire was born March 16th 1988 and has received his first degree in the Field of Applied Biology and obtained Bachelor of Science Degree in Biology (In Microbiology and Parasitology specialization) from the University of Ambo, Ethiopia in June 24th 2010. He has obtained a Master of Science in the field of applied Microbiology from Addis Ababa University, Ethiopia in July 2012. He has also received an International Master of Science in the field of Molecular Medicine from Norwegian University of Science and Technology, Norway in June 12th 2017. He is expertise in Microbiology, Parastiology and Oncology. He has served as an instructor and researcher at the Dilla University, Ethiopia for three years since July 8th 2012- July 9th 2015.
Abstract:
Norwegian University of Science and Technology, Faculty of Medicine and Health Sciences, Department of Cancer Research and Molecular Medicine, Trondheim, Norway.
Follistatin-like 5 (FSTL5) is an 847-amino acid, suggested secretory glycoprotein. The FSTL5 gene is composed of sixteen exons and the gene’s function is little known. FSTL5 is expressed by some myeloma cells and the gene has been suggested to play a role in multiple myeloma. Thus, the aim of this thesis was to find out more about FSTL5 expression and function in myeloma cells. In order to achieve our objectives, we have used these methods: Western blot, flow cytometry, and real time PCR quantification. Inhibitors of translation and autophagy, inhibitors of pathways positive for myeloma cell growth and survival, and different growth conditions were used to investigate the regulation of FSTL5 protein expression in myeloma cell lines. By Western blotting, we found two different protein bands that likely corresponded to FSTL5 protein. In general, conditions that were negative for the cell’s survival induced higher levels of a short variant of FSTL5 protein expression in myeloma cell lines. The increase in the short variant of FSTL5 during apoptotic conditions was inhibited by a general caspase inhibitor. We were not able to see a clear correlation between mRNA levels of FSTL5 and FSTL5 protein in a panel of myeloma cell lines. In conclusion, these results indicated that levels of a short variant of FSTL5 protein correlated negatively with cell viability and that the presence of this shorter variant was dependent on caspase activity. The actual function of FSTL5 in myeloma cells still remains to be shown.
